Hysterectomy
When medication and other treatments are unable to relieve symptoms, hysterectomy is often recommended to provide a more effective, definitive and long-term solution for excessive menstrual bleeding. If you are considering or your doctor has recommended a hysterectomy, you are not alone - one in three women in the U.S. will have a hysterectomy before turning 60.
Physicians perform hysterectomy – the surgical removal of the uterus – to treat a wide variety of uterine conditions. Each year in the U.S. alone, doctors perform approximately 600,000 hysterectomies, making it the second most common surgical procedure for women.
Types of Hysterectomy
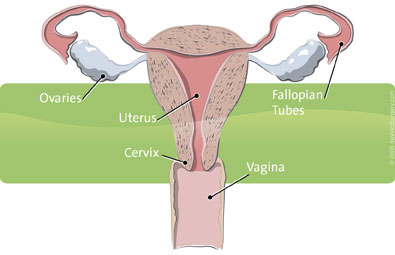
There are various types of hysterectomy that are performed depending on the patient’s diagnosis. All hysterectomies involve removal of the uterus. What can vary are which additional reproductive organs and other tissues that may be removed. Types of hysterectomy include:
- Partial or subtotal hysterectomy: This is also known as a supracervical hysterectomy. This procedure involves removing the uterus, but leaves the cervix intact. This decision is often based upon patient preference. Some women feel that leaving the cervix intact will preserve sexual function following surgery.
- Total hysterectomy: This procedure involves removing the uterus and the cervix. The vagina remains entirely intact. This is the most common type of hysterectomy performed.
- Removal of lymph nodes: For hysterectomies performed for malignant conditions – such as uterine, cervical, or ovarian cancer – the surgeon will also remove certain lymph nodes. This procedure is often referred to as a lymph node dissection or lymphadenectomy. Lymph nodes will be removed in certain areas, depending upon the location and extent of the disease. Lymph node removal also helps your surgeon determine the extent or stage of your cancer, and can guide further adjuvant treatment, such as radiation therapy or chemotherapy.
- Removal of the fallopian tubes and ovaries: These organs may or may not be removed during your hysterectomy procedure. This will depend upon your condition, age, and other factors. Often, the ovaries and fallopian tubes are left intact.3 Removal of the ovaries is called an oophorectomy. Removal of fallopian tubes and ovaries is called a salpingo-oophorectomy.
- Radical hysterectomy: Removes the uterus and cervix
- Total hysterectomy: This procedure is most often performed for cervical cancer, and involves removal of the uterus, tissues next to the uterus, the upper part (about 1 inch) of the vagina and pelvic lymph nodes. The fallopian tubes and ovaries may also be removed.
Approaches to Hysterectomy
Surgeons perform the majority of hysterectomies using an “open” approach, which is through a large abdominal incision. An open approach to the hysterectomy procedure requires a 6-12 inch incision.
A second approach is vaginal hysterectomy, which involves the removal of the uterus through the vagina, without any external incision or subsequent scarring. Surgeons most often use this minimally invasive approach if the patient’s condition is benign, when the uterus is normal size and the condition is limited to the uterus.
In laparoscopic hysterectomies, the uterus is removed using instruments inserted through small tubes into the abdomen, resulting in 3-5 small incisions in the abdomen. One of these instruments is an endoscope – a small miniaturized camera – which allows the surgeon to see the target anatomy on a standard 2D video monitor. A laparoscopic approach offers surgeons better visualization of affected structures than either vaginal or abdominal hysterectomy.
You may encounter shorthand abbreviations describing different approaches to hysterectomy. Some of these are as follows:
- Total Laparoscopic Hysterectomy (TLH): The uterus and cervix are removed using laparoscopic instrumentation through 3-5 small incisions made in the abdomen.
- Laparoscopic Supracervical Hysterectomy (LSH): The uterus is removed, but the cervix is left in tact, using laparoscopic instrumentation through 3-5 small incisions made in the abdomen. The uterus is removed through one of the small incisions using an instrument called a morcellator.
- Total Vaginal Hysterectomy (TVH): The uterus and cervix are removed through an incision deep inside the vagina. This is often the surgical approach to treat uterine prolapse.
- Total Abdominal Hysterectomy (TAH): The uterus and cervix are removed through a large abdominal incision. The incision size can vary from 6-12 inches, depending upon the patient’s condition.
While minimally invasive vaginal and laparoscopic hysterectomies offer important potential advantages to patients over open abdominal hysterectomy – including reduced risk for complications, a shorter hospitalization and faster recovery – there are inherent drawbacks. With vaginal hysterectomy, surgeons are challenged by a small working space and lack of view to the pelvic organs. Additional conditions can make the vaginal approach difficult, including when the patient has:
- A narrow pubic arch (an area between the hip bones where they come together)
- Thick adhesions due to prior pelvic surgery, such as C-section
- Severe endometriosis
- Non-localized cancer (cancer outside the uterus) requiring more extensive tissue removal, including lymph nodes
With laparoscopic hysterectomies, surgeons may be limited in their dexterity (since the instruments are straight and rigid) and by 2D visualization, both of which can potentially reduce the surgeon's precision and control when compared with traditional abdominal surgery.
da Vinci Hysterectomy
One in three women in the U.S. will have a hysterectomy before she turns 60.1 While no woman wants to face surgery, today the vast majority of gynecologic conditions - from endometriosis to uterine fibroids, heavy menstrual bleeding to cancer - can now be treated effectively without a big incision. With da Vinci® Surgery, a hysterectomy requires only a few small incisions, so you can get back to life faster - within days rather than the usual weeks required with traditional surgery.
da Vinci Surgery enables gynecologists to perform the most precise, minimally invasive hysterectomy available today. For most women, da Vinci Hysterectomy offers numerous potential benefits over traditional open surgery, including:
- Significantly less pain
- Minimal blood loss and need for transfusion
- Fewer complications
- Shorter hospital stay
- Quicker recovery and return to normal activities
- Small incisions for minimal scarring
- Better outcomes and patient satisfaction, in many cases
Surpassing the limits of conventional laparoscopic surgery, da Vinci is revolutionizing gynecologic surgery for women. No wonder more and more women are choosing da Vinci Surgery for their hysterectomy.
If you have been putting off surgery to resolve a gynecologic problem, it may be time to ask your doctor about da Vinci Surgery.
Learn why da Vinci Hysterectomy may be your best treatment option. While clinical studies support the effectiveness of the da Vinci® System when used in minimally invasive surgery, individual results may vary. Surgery with the da Vinci Surgical System may not be appropriate for every individual. Always ask your doctor about all treatment options, as well as their risks and benefits.
